 Overview
OverviewHammer, mallet, and claw toes have distinctive differences that can assist you in determining what kind of toe problem you are dealing with. All three conditions deal with toes that are curved into abnormal positions, which possibly look strange and may cause pain. Typically, the big toe is not affected by these problems. A Hammer toe tends to bend downward at the center of a toe joint. It generally affects your second toe. The affliction causes the center of your toe to rise and is often accompanied with a bony lump.
Causes
Wearing shoes that squeeze the toes or high heels that jam the toes into the front of the shoe. Other causes or factors in the development of hammertoes can include an injury such as badly stubbing your toe, arthritis and nerve and muscle damage from diseases such as diabetes. And, hammertoes tend to run in families, although it is more likely the faulty foot mechanics that lead to hammertoes that are inherited, not the hammertoes themselves. Hammertoe generally affect the smaller toes of the foot, especially the second toe, which for many people is the longest toe. It's uncommon for the big toe to be bent this way.
 Symptoms
SymptomsPain on the bottom of your foot, especially under the ball of your foot, is one of the most common symptoms associated with hammertoes. Other common signs and symptoms of hammertoes include pain at the top of your bent toe from footwear pressure. Corns on the top of your bent toe. Redness and swelling in your affected area. Decreased joint range of motion in your affected toe joints.
Diagnosis
Some questions your doctor may ask of you include, when did you first begin having foot problems? How much pain are your feet or toes causing you? Where is the pain located? What, if anything, seems to improve your symptoms? What, if anything, appears to worsen your symptoms? What kind of shoes do you normally wear? Your doctor can diagnose hammertoe or mallet toe by examining your foot. Your doctor may also order X-rays to further evaluate the bones and joints of your feet and toes.
Non Surgical Treatment
If your hammertoe problem is diagnosed as flexible hammertoe, there are a number of nonsurgical treatments that may be able to straighten out your toe or toes and return them to their proper alignment. Padding and Taping. Your physician may pad the boney top-part of your hammertoe as a means of relieving pain, and may tape your toes as a way to change their position, correct the muscle imbalance and relieve the pressure that led to the hammertoe's development. Medication. Anti-inflammatory drugs such as aspirin and ibuprofen can help deal with inflammation, swelling and pain caused by your hammertoe. Cortisone injections may be prescribed for the same purpose. If your hammertoe is a consequence of arthritis, your physician may prescribe medications for that.
Surgical Treatment
The technique the surgeon applies during the surgery depends on how much flexibility the person's affected toes still retain. If some flexibility has still been preserved in their affected toes, the hammer toes might be corrected through making a small incision into the toe so the surgeon can manipulate the tendon that is forcing the person's toes into a curved position. If, however, the person's toes have become completely rigid, the surgeon might have to do more than re-aligning the person's tendons. Some pieces of bone may have hammertoe to be removed so the person's toe has the ability to straighten out. If this is the case, some pins are attached onto the person's foot afterwards to fix their bones into place while the injured tissue heals.
 Prevention
PreventionIn some cases foot problems may present at birth, many foot problems such as hammer toes can be prevented. Hammer toe prevention can be a simple process, such as, checking your feet regularly and wearing the right shoes for your feet. Good circulation is also an essential part of foot health and hammer toe prevention. Taking a warm foot bath or giving yourself a foot massage are great ways of keeping your feet healthy.
 Overview
Overview Symptoms
Symptoms Prevention
Prevention



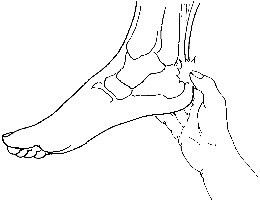
 Tendinitis is inflammation of a tendon. Thus, Achilles tendinitis is an inflammation of the Achilles tendon. The inflammation may be localized to the end of the tendon closest to the heel or may spread upward to affect even the muscles of the calf. Swelling often occurs and pain is felt upon contraction of the calf muscles. In severe cases, pain may be felt even at rest. Generally, Achilles tendinitis begins as a dull pain at the back of the lower leg just above the heel when pushing off the ground with the foot. Unless the activity is stopped, the condition rapidly gets worse until any activity requiring a push-off from the ground by the foot becomes quite painful and nearly impossible. If it is left untreated, it can develop into one of two more serious conditions - Achilles tendinosis and Insertional Calcific Tendinitis.
Tendinitis is inflammation of a tendon. Thus, Achilles tendinitis is an inflammation of the Achilles tendon. The inflammation may be localized to the end of the tendon closest to the heel or may spread upward to affect even the muscles of the calf. Swelling often occurs and pain is felt upon contraction of the calf muscles. In severe cases, pain may be felt even at rest. Generally, Achilles tendinitis begins as a dull pain at the back of the lower leg just above the heel when pushing off the ground with the foot. Unless the activity is stopped, the condition rapidly gets worse until any activity requiring a push-off from the ground by the foot becomes quite painful and nearly impossible. If it is left untreated, it can develop into one of two more serious conditions - Achilles tendinosis and Insertional Calcific Tendinitis.








 RSS Feed
RSS Feed